United for Global Mental Health
Lessons and Recommendations from the World’s Largest Gathering on Mental Health Advocacy
Multistakeholder Collaboration
10 Feb 2026
Mansi Chopra, Mona Balani | 23 Sep 2025
This article is part of the Lived Experience Perspectives Series, which features firsthand accounts from individuals living with noncommunicable diseases, mental health, or neurological conditions. Each piece highlights one of the key advocacy messages from the WHO Symposium on the Meaningful Engagement of People Living with NCDs, Mental Health, and Neurological Conditions , contributing to global advocacy efforts in the lead-up to the Fourth High-Level Meeting of the UN General Assembly on NCDs and Mental Health in September 2025.
This article highlights Key Advocacy Message 4.3:
To invest in strengthening and resourcing meaningful engagement by supporting research initiatives that strengthen the evidence base for meaningful engagement.
We are caregivers. From a young age, we both have been looking after grandparents, parents, in-laws, partners and children living with chronic illnesses. Diabetes, hypertension, cardiovascular diseases, chronic kidney disease, Chronic Obstructive Pulmonary Disease, arthritis, tuberculosis, HIV/AIDS and other health conditions have deeply affected our families and households. Over time, we have lost loved ones and in Mona’s case, even her partner and child.
In technical terms, caregiving describes providing ongoing support for health and daily living for people living with chronic conditions. For us, in practice, it has been a major challenge that is often carried out unrecognized and in silence. We are balancing caregiving with motherhood, widowhood, and working full-time.
As caregivers, we have navigated hospital corridors during emergencies, faced stigma and emotional distress, managed in-house clinical set-ups, and watched family members cycle through fragmented care pathways. Whether it was coordinating dialysis and heart treatment across separate hospitals or shuttling between specialists for multiple co-morbidities, we have consistently faced misdiagnoses, long waiting times, financial strain, disease management distress, and a lack of empathy within the health system, while quietly holding our families together. Yet, no one thought to ask what we may need in terms of support. Our lived experience of providing care for loved ones seemed to count very little.
Too often, caregivers remain at the periphery of healthcare. We are among the first to spot inefficiencies in proving care and to imagine practical improvements; that is why our lived experience cannot be dismissed as anecdotal. It is this experiential evidence that can transform health systems.
Caregiving is itself a form of lived experience. As caregivers spend sustained time with their family members or with people living with chronic conditions, they observe daily management and care routines, build practical knowledge that complements clinical data, and observe first-hand how healthcare requires strengthening at the point of delivery.
When caregivers are included in decision-making and leadership processes, they can bring these concrete insights and practical solutions to the table and help strengthen health system performance and more inclusive health policies and programmes.
Health does not exist in isolation, and neither should our response strategies. Social, economic and environmental determinants shape health outcomes, so moving away from vertical, fragmented programmes toward horizontal, integrated multisectoral action is essential. Including caregivers’ perspectives in programme design not only ensures the complex realities faced by people living with chronic conditions and their caregivers are reflected, but it is also a means to redistribute power and build people-centered health systems.
In several projects undertaken in our professional capacity, community conversations, in-depth interviews, small-group meetings and workshops with people living with chronic conditions and their caregivers have helped identify barriers and enablers of healthcare access and co-develop practical, local solutions.
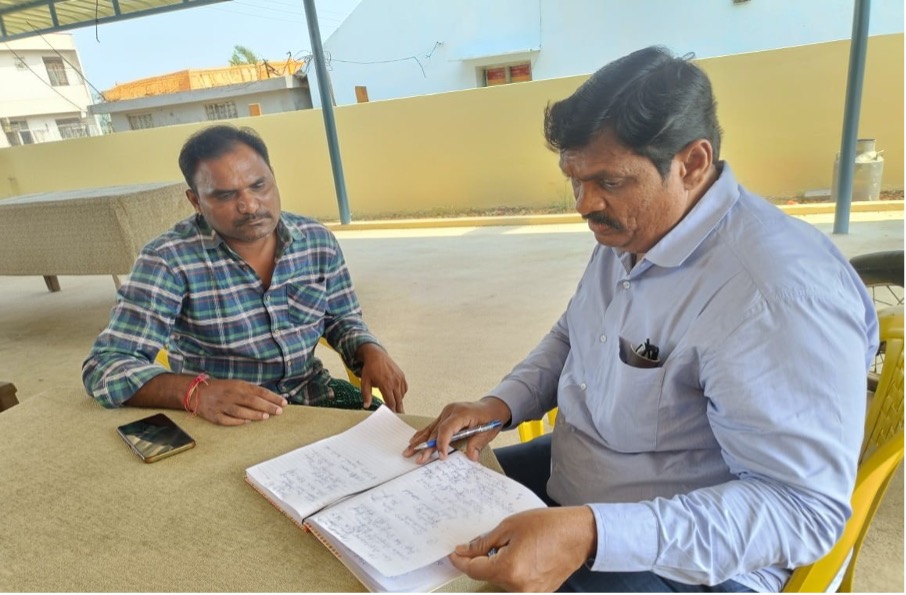
For example, in Marripalem village, Andhra Pradesh, Gavireddy Siva (36) lives with diabetes and hypertension and has been a caregiver for his father for almost a decade. He shared how self-stigma, taking medications in public, and out of pocket expenditure for medication for his father and himself initially prevented them from seeking care. These experiences have informed a response by HRIDAY, including training people with lived experience and caregivers to establish local peer-support groups and networks, community advisory boards, and co-create culturally resonant awareness activities.

These activities cover self-management, stigma reduction, early screening, health system navigation, and treatment adherence. Culturally resonant awareness activites include short street plays, folk songs, information, education and communication resources, as well as implementation briefs and micro-documentaries in local languages. Success stories of these community activites and their champions are being documented through participatory, community-led approaches that are inspiring change beyond individual villages.

There are moments from our experience as caregivers that remain etched in our memory because of the challenges we faced to seek treatment. These moments continue to fuel our belief that research grounded in the principles of meaningful community engagement is essential to build systems that are not only person-centered, inclusive, and equitable, but also trusted, responsive, and sustainable.
As we approach the UN High-Level Meeting on NCDs and Mental Health in September 2025, we are reminded that lasting, transformative change must be rooted in real experience and anchor our appeal aligned to the WHO Symposium on Meaningful Engagement Key Message: “Invest in research and capacity building for meaningful engagement”. This means strengthening the skills of people with lived experience and, in particular, caregivers to take active roles in co-designing, implementing, and monitoring health responses, while also ensuring that participatory research is funded, respected, and acted upon.
To move from tokenism to true transformation, community-led, participatory research must be embedded in and funded through national strategies. Funders must treat meaningful engagement as a core requirement, and academic institutions should revise ethics and authorship norms to include lived experience voices as equal partners.
We must shift the paradigm from one where people with lived experience and caregivers, like us, are studied, to one where we co-create and lead research agendas, shape advisory boards, influence ethics reviews, and co-create change.

Mansi Chopra
Dr. Mansi Chopra is a caregiver and a public health researcher, dedicated to advancing meaningful engagement, equity and empathy in healthcare research and policy action in low-and middle-income countries. Her work spans community engagement, noncommunicable disease (NCD) prevention, management, and control, and systems strengthening, with a focus on co-creating people-centered responses for NCDs and multiple long-term conditions. She has contributed to shaping global agendas on meaningful engagement through the WHO Global Coordination Mechanism for NCDs and serves on the Steering Committee of the WHO Symposium on Meaningful Engagement of People Living with NCDs, Mental Health and Neurological Conditions. As Director (Research) at HRIDAY, Dr. Chopra leads initiatives that amplify the voices of communities, caregivers, and people with lived experience in research, policy, and capacity building. Her work, published in leading journals and global reports, advances inclusive, compassionate, equitable, empathic, and evidence-based approaches to health, ensuring that those most affected are at the centre of decision-making.
Mona Balani
Mona Balani is a social worker, caregiver, and public health professional from India with nearly two decades of experience leading community-driven health initiatives. A long-term survivor living with HIV for more than 25 years, she has become a powerful advocate for HIV, TB, and NCDs, championing equity, empathy, and meaningful engagement of people with lived experience. Her work spans from grassroots mobilization to national policy influence, with a focus on strengthening community systems and embedding accountability through community-led monitoring. She serves as a technical expert with the National Human Rights Commission (NHRC), contributes to committees under NACO and the National Health Mission (NHM), and advises on women’s and children’s health. Internationally, she has worked with UNAIDS, WHO, and the Central TB Division on the End AIDS Agenda 2030, while also advocating for integrated, person-centered care models that address HIV, TB, Hepatitis C, cervical cancer, and NCDs.