World Diabetes Foundation
Heroes of remote Nepal: Women leading the way to healthier communities
25 Oct 2024
WHO Regional Office for South-East Asia | 15 Feb 2024
Childhood cancer is an important cause of childhood disease burden. It is curable with affordable care in vast majority of cases. About 1,500 - 2,000 new childhood cancer cases are estimated to occur every year in Myanmar. There are two hospitals providing comprehensive childhood cancer services in the country. Yangon Children’s Hospital (YCH), located in Yangon city, provides services to patients mostly from southern part of Myanmar and Mandalay Children’s Hospital (MCH), located in Chanayethazan township, provides services to patients from remaining parts of Myanmar. The need for travel to a faraway city for treatment of a child adds significantly to the burden on families. This is a common situation in many other low- and middle-income countries.

Currently, 700 - 800 new children are diagnosed with cancer annually in Myanmar, with more than 400 patients getting treatment at Yangon Children’s Hospital. Around 75% of cases in Yangon Children’s Hospital are referred from outside Yangon city. Similar is the scenario with Mandalay Children’s Hospital. Many of the children with cancer are from poor socio-economic status, which often interferes in adherence with treatment schedule and completion. Over 15% of the newly diagnosed children with cancer abandon treatment within first year in Myanmar. The need for frequent travel to or stay in the city of primary treatment center is one contributor to the financial hardships.
Children with cancer receiving treatment at Yangon or Mandalay, who face difficulty staying in the city for the entire duration of treatment, are sent to their home at certain points during their treatment courses. This happens, for example, during treatment cycles break or during phases requiring only low intensity oral medication. They are advised to seek care at health facilities nearby their home in case of any emergency. They have to return to Yangon or Mandalay for the following cycle of treatment, for monitoring and prescribing for the following month, or when there are complications. This requires patient and families to frequently travel to the city of primary treatment center, also causing delays in many instances. An innovative service delivery approach was thus needed to provide services closer to patient’s home.
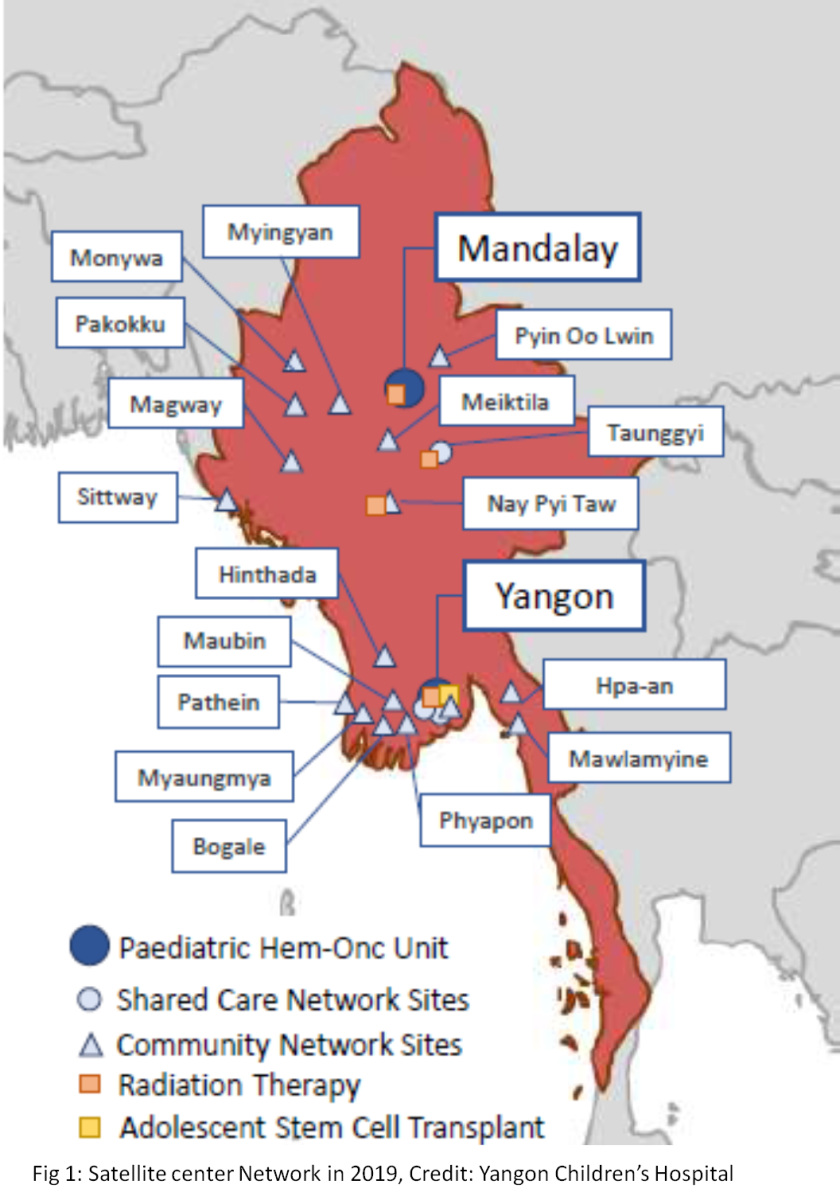
To mitigate this, in 2019, Yangon Children’s Hospital and Mandalay Children’s Hospital established collaboration with hospitals at lower levels of care, the satellite hospitals. Five satellite sites were linked to MCH and 12 sites to the YCH (Figure 1).
The collaboration with a new satellite site was typically initiated with a call for collaboration from the principal treatment center when there was a need for referring patients to the potential satellite site. Availability of pediatrician with interest in taking up the task was set as the most important factor in selection of a potential site. Healthcare staffs at satellite center were trained on basic pediatric oncology including the diseases, treatment regimens, handling of chemotherapy medicines, oncologic emergencies etc to build their capacity to deliver relatively less complicated part of care for children receiving cancer treatment. The pediatrician in satellite center was informed in detail about the patient and the treatment plans via telephone prior to referral. Transportation for such patients was specially arranged, mechanism was established for supply of medicines to the satellite center. A patient book was developed that was carried by the patient. The treatment details were recorded by the primary as well as the satellite site in the same patient book. Important information on diagnosis and treatment were also recorded in computer at the principal treatment center when the patient visited there. Arrangements were made for review and monitoring of patient’s progress via periodic and need based virtual meetings between principal treatment center and satellite center. This arrangement of satellite center network was endorsed by the pediatric society.
With the families having freedom of choice, services utilization at satellite site network hospitals was not very high in the beginning. However, with the increasing impact of COVID-19 pandemic in 2020, when people’s movement and transport were severely restricted, the satellite center network hospitals throughout the country were increasingly utilized by the families and the centers played an important role to ensure treatment continuity. Total 311 patients were referred from YCH to 25 hospitals in 7 states/regions between August – December 2020.
WHO Global Initiative for Childhood Cancer (GICC) was launched by WHO in 2018 along with St. Jude Children’s Research Hospital and other partners with the aim of achieving at least 60% global survival and reducing suffering for all children with cancer by 2030. WHO Regional office for South-East Asia has three GICC focus countries including Myanmar and has established South-East Asia Regional Childhood Cancer Network (SEAR-CCN) to foster collaboration among institutions in improving quality and coverage of care for childhood cancer.
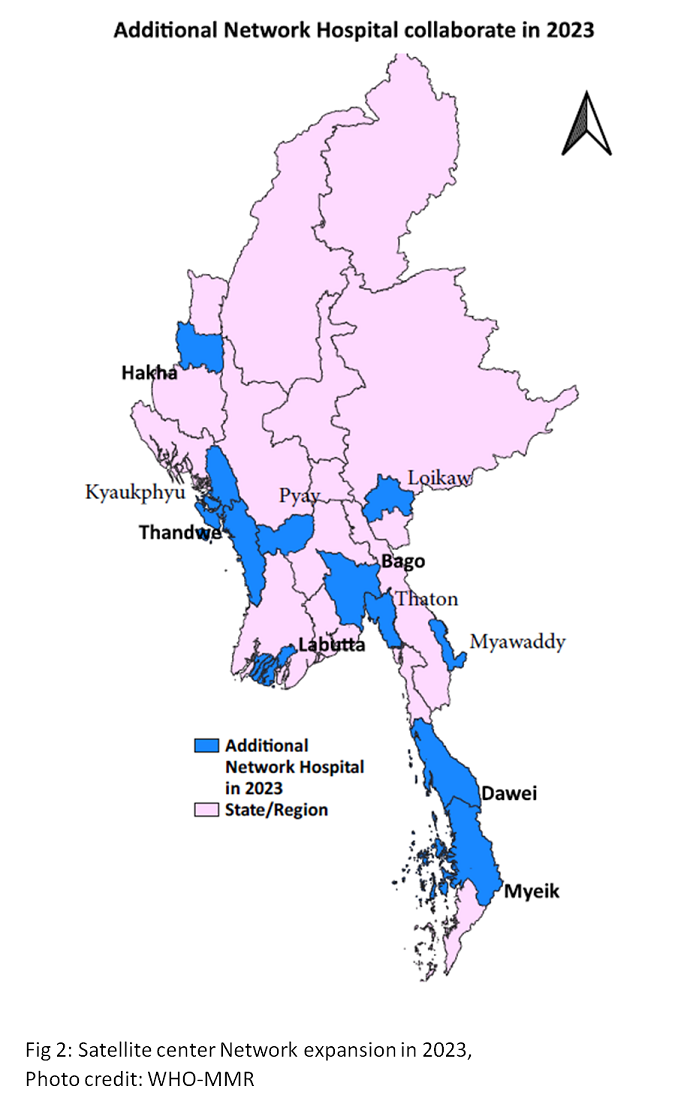
 Yangon Children’s Hospital was nominated by the Ministry of Health to participate in SEAR-CCN and lead the change working along the global initiative.Yangon Children’s Hospital actively participated in the network activities and increased collaboration with fellow institutions. One such collaboration involved that with Kati Children’s Hospital in Nepal, by way of which the two hospitals shared the experiences of leading similar initiatives in similar circumstances benefiting both. GICC continued support to the Myanmar initiative. The number of satellite center network hospitals increased from 17 in 2019 to 41 in 2023. Figure 1 & 2 show network hospitals identified in 2019 and additional network hospitals collaborating in 2023 respectively.
Yangon Children’s Hospital was nominated by the Ministry of Health to participate in SEAR-CCN and lead the change working along the global initiative.Yangon Children’s Hospital actively participated in the network activities and increased collaboration with fellow institutions. One such collaboration involved that with Kati Children’s Hospital in Nepal, by way of which the two hospitals shared the experiences of leading similar initiatives in similar circumstances benefiting both. GICC continued support to the Myanmar initiative. The number of satellite center network hospitals increased from 17 in 2019 to 41 in 2023. Figure 1 & 2 show network hospitals identified in 2019 and additional network hospitals collaborating in 2023 respectively.
Sustaining progress amidst the crisis
In 2021 due to change in the political situation in the country, several trained health workforces moved out from the service. Added onto the impact of COVID19 pandemic, the priority childhood cancer service was reduced to very low. The burden on families of children with cancer worsened further due to the ensuing economic impact on the country and the families. Thus, more patients opted to obtaining care at satellite hospitals. Closer to the end of 2022, WHO supported in recruitment of staffs and supply of essential medicines for continuity of childhood cancer services. Following which collaboration with network hospitals became more active, patient review meeting revitalized, satellite center resource guides development continued, training to healthcare providers were continued virtually, and supply of essential medicine were sustained.
The occurrence of cyclone Mocha came as another instance demonstrating the utility of the satellite center network in providing resilience at times of crisis. Patients seeking care from satellite sites saw a rise in cyclone hit areas.
During COVID 19 pandemic, the political crisis, and the aftermath of cyclone Mocha a total 115 health care providers from 41 network hospitals at 15 State/Region were trained virtually on pediatric oncology virtually. Medication information booklet and early warning signs pamphlet were also delivered to the network hospitals.
Total 907 patient reviews were carried out through 9 sessions of review meeting with 22 network hospitals from 13 state/regions between November 2022 to December 2023. Of 491 new cases diagnosed in Yangon children’s hospital in 2023, 32% of patients were jointly treated with YCH and network hospitals. Some satellite centers have taken more patients compared to others but none of the satellite center has stopped functioning till date.
Although childhood cancer is highlz curable, the survival rate is as low as 20% in low-or middle income countries. Every child with cancer deserves better care and a better life. With small and strategic investment, it could save millions of children over the next decade. That is why, as part of giving a better chance of life for children with cancer, WHO supported the Childhood Cancer Initiative in Myanmar with the commitment to level these inequalities.
Dr. Thushara Fernando, WHO Representative to Myanmar
Shared care with satellite site network hospitals is a remarkable model in bringing the services closer to the home of children with cancer. And this significantly improves resilience at times of crisis. Continuing technical support and mentoring from principal treatment center and provision of reliable supply of essential medicines is crucial to ensure success of the model. Increasing engagement, ownership, and facilitation from government in functioning of the satellite center network indicates the usefulness and progress towards sustainability of this model in Myanmar. In the South-East Asia Region, this model of care has been in implementation in Myanmar and Nepal. The comparison in outcome between the groups utilizing this model with those receiving treatment only from the principal treatment center will be the next essential step in building evidence in favor of this model.