International League of Dermatological Societies
Addressing Dermatological Needs and Challenges in Lebanon's Refugee and Local Communities
Meaningful Engagement of People with Lived Experiences
20 Jul 2023
World Health Organization. Regional Office for the Eastern Mediterranean | 12 Sep 2023
Lebanon was already facing crises before the COVID-19 outbreak, including economic collapse and the world’s highest number of refugees per capita. The Beirut Port explosion in August 2020 further devasted the country’s economy. Despite all this, Lebanon has taken effective steps to combat noncommunicable diseases (NCDs), which are responsible for approximately 91% of all deaths in the country.
 Over the last decade, Lebanon has implemented a major reform of its mental health system, making it more resilient to emergencies such as the COVID-19 pandemic.
Over the last decade, Lebanon has implemented a major reform of its mental health system, making it more resilient to emergencies such as the COVID-19 pandemic.
Lebanon has developed a nutrition strategy to achieve greater food security and build resilience. The strategy is informed by extensive surveillance of the country’s food security situation.
The chronic medications programme, run in collaboration with YMCA, has improved access to quality NCD medications for both Lebanese nationals and Syrian refugees.
Lebanon introduced a ban on public waterpipe use and increased access to tobacco cessation services during the pandemic.
In 2016, cancer accounted for 27.2% of all NCD-related premature deaths, but many Lebanese hospitals lack palliative care services. Lebanon has begun bridging this gap by working with SANAD, a non-profit nongovernmental organization specializing in home-based hospice care.
The Ministry of Public Health collaborated with WHO, Rafik Hariri University Hospital and other stakeholders to invite SANAD to set up and train a palliative care team in Rafik Hariri University Hospital. The team of 36 physicians, nursing supervisors, nurses, pharmacists and social workers have delivered high-quality palliative care services, working closely with the hospital’s oncology departments.
The result is an accessible, affordable service with high patient and caregiver satisfaction, which proves that palliative care can be integrated into large public hospitals in Lebanon. The Ministry of Public Health is building on this success, with WHO support, by expanding the programme to Ain Wazein Hospital and inviting SANAD to train an outreach team to deliver community palliative care services.
Lebanon has developed its first National Nutrition Strategy and Action Plan (2021–2026). WHO Lebanon led the development of the strategy, consulting with key stakeholders including the ministries of Public Health, Agriculture, Economy and Trade throughout the process.
The strategy is vital, as the country is going through a nutrition transition from a traditional, varied diet towards more “western” high-calorie, highly processed, lower fibre foods. The result is a “double burden of malnutrition” where undernutrition affects some parts of the population, while others suffer from obesity. Food insecurity has been affected by the multiple crises that have hit Lebanon since 2019. Not least, the destruction of the Port of Beirut, along with much of the country’s grain reserves, which closed the entry point for around 60% of Lebanon’s food imports.
Surveillance is being used to inform the nutrition strategy. The Nutrition Assessment System is a mobile app that was used to collect data between November 2020 and March 2021. It revealed that more than 70% of households in Lebanon skip meals to spare food. Using the Arab Family Food Security Scale, 75.4% of households are severely food insecure. Meanwhile, the percentage of respondents who reported being below the poverty line tripled from 4.6% before the pandemic to 13.5% since the outbreak.
This information is informing the evidence-based strategy for food security interventions, with the aim of building more resilient households, communities, and food systems for the future.
Lebanon has been working to reduce its high rates of tobacco use since ratifying the WHO Framework Convention on Tobacco Control (WHO FCTC) in 2005. A long-running campaign by numerous stakeholders, including the National Tobacco Control Programme, led to the passing of Law 174 in 2011, which made Lebanon smoke free.
These steps made it easier for Lebanon to implement a ban on the use of waterpipes in public places during the pandemic. The waterpipe ban was led by the Ministry of Public Health and enforced with heavy fines by the Ministry of Interior and the Ministry of Tourism.
At the same time, the Ministry of Public Health set up a tobacco cessation helpline and worked with seven cessation centres across Lebanon to help people quit tobacco.
In 2014, the Ministry of Public Health created the National Mental Health Programme to reform the country’s mental health system and scale up services by merging humanitarian and development agendas. The programme launched the Mental Health and Substance Use Strategy for Lebanon 2015–2020, with the goal of re-orientating services towards a cost-effective community-based model.
The Mental Health and Substance Use Strategy included seven cost-effective and evidence-based interventions:
The last of these interventions delivers collaborative stepped-care mental health services through a supportive network of specialists at 27 primary health care (PHC) centres across Lebanon. This is essential in a country where 30% of the total population are refugees, many of whom have mental health burdens and are less able to access mental health care in refugee camps.
The Ministry of Public Health is also leading the Mental Health and Psychosocial Support Task Force. This includes more than 60 organizations working on the Syrian crisis response in Lebanon, with the aim of improving access to care while harmonizing and mainstreaming mental health and psychosocial support in all sectors.
The United Nations Relief and Works Agency for Palestine Refugees in the Near East (UNRWA) started training multidisciplinary staff in mental health and psychosocial support in 2013. It began a full integration of mental health and psychosocial support services in its primary health care centres from 2017. As well as providing training for staff such as doctors, nurses, midwives and pharmacists, the programme includes:
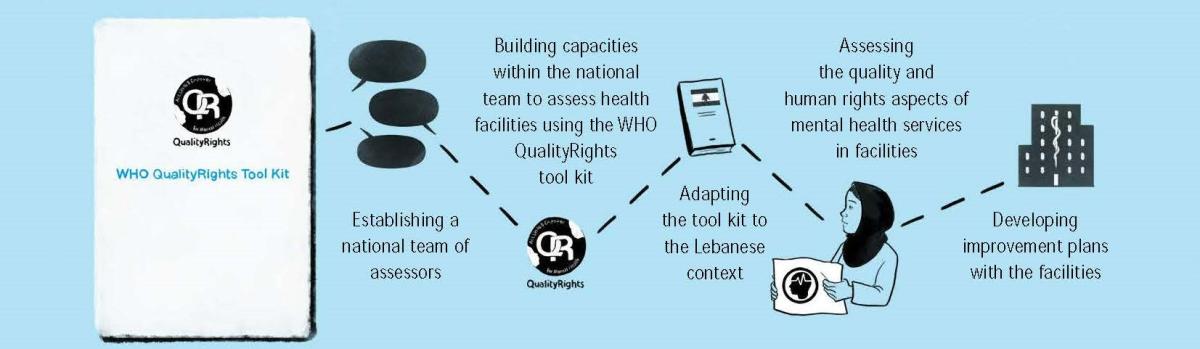
The move to improve the quality and human rights aspect of mental health services by using the WHO QualityRights tool kit has seen the successful engagement of the private health care system. Core elements of the intervention included:
The Ministry of Social Affairs is represented on the national assessment team. The Ministry’s involvement is essential in the successful implementation of the project and its potential scaling-up to different types of facilities.
Every aspect of the successful reform of mental health services has relied on strong multi-level, intersectoral collaboration. By addressing mental health as a priority, Lebanon is in a much better position to deal with the psychological shocks of emergencies. This fact can be seen clearly in its response to the COVID-19 pandemic.
The National Mental Health Programme developed a national action plan with WHO and UNICEF to ensure continuity of mental health care, while supporting the mental health of people in quarantine, their families and health care workers. Actions included:
Following its work over the last decade and throughout the pandemic, Lebanon can take all its experience forward as it continues to respond to the mental health needs of its citizens and refugees.
This country story is part of a series on sharing successful strategies from the Eastern Mediterranean Region mitigating noncommunicable diseases and mental health disorders during the COVID-19 pandemic and beyond. Discover additional stories and insights in the full report published by the World Health Organization Regional Office for the Eastern Mediterranean.