WHO Regional Office for Africa
Ensuring primary health services for displaced people
27 Sep 2024
World Health Organization. Regional Office for the Eastern Mediterranean | 11 Sep 2023
Noncommunicable diseases (NCDs) account for 52% of deaths in Sudan, but addressing the burden of NCDs is not straightforward. Sudan is home to over 1.2 million refugees, and geographic, demographic and financial factors add to the complexity of the country’s NCD burden. However, through strong collaboration across government departments and with nongovernmental organizations, international agencies and foreign governments, Sudan has improved NCD service provision during the COVID-19 pandemic.
 Sudan took multisectoral action to ensure the provision of mental health and psychosocial support services during the pandemic, both at state and federal levels.
Sudan took multisectoral action to ensure the provision of mental health and psychosocial support services during the pandemic, both at state and federal levels.
Sudan, the United Nations High Commissioner for Refugees (UNHCR) and WHO worked together to integrate mental health and psychosocial support services within humanitarian assistance programmes and build health care capacity in the country.
The Federal Ministry of Health collaborated with WHO to deliver telemedicine services during the pandemic to replace face-to-face services.
Sudan banned the public use of waterpipes during the pandemic and worked with international agencies and nongovernmental organizations to create an awareness campaign linking smoking and COVID-19.
Organizations including the Sudan Heart Society and the Sudanese American Medical Association created the “SUR I CAAN” framework to diagnose and treat rheumatic heart disease, raise awareness and train health workers.
Sudan has a high burden of rheumatic heart disease. To address this problem, experts from the Sudan Heart Society, the Sudan Association of Paediatricians and the Sudanese American Medical Association have collaborated to create the “SUR I CAAN” framework.
This is based on:
Collaboration with multiple partners, including the Sudanese Children’s Heart Society and Miraglo, has been key to the framework’s success. The Federal Ministry of Health is now looking to incorporate rheumatic heart disease-specific activities into the NCD package and prioritize PHC-level interventions to ensure accessibility.
Sudan banned the use of waterpipes in March 2020. The accompanying awareness campaign was co-funded by and implemented with a range of international agencies and nongovernmental organizations.
The campaign included:
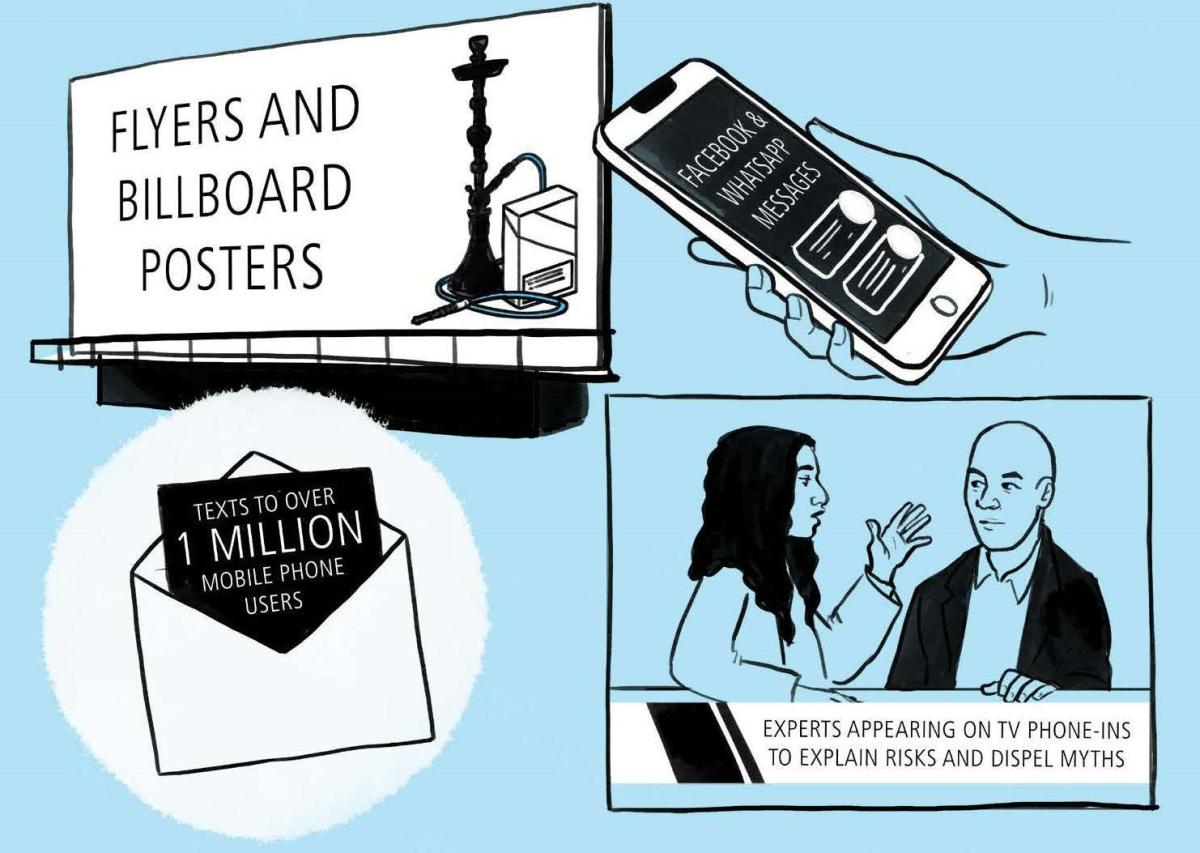
Sudan intends to continue the waterpipe ban after life returns to “normal”, continue health warnings on cigarette packs, and enact a comprehensive ban on tobacco advertising.
The COVID-19 pandemic severely disrupted health services, especially at primary health care (PHC) level, which is the access point for most NCD patients. Cancer care and kidney dialysis services were also interrupted. The Federal Ministry of Health worked closely with WHO and over a dozen stakeholders to implement a range of responses.
Telemedicine was a vital component of these responses. PHC physicians were rapidly trained to provide telephone consultations and complete electronic patient records through the primary care helpline. The helpline offered:
Physicians could also refer patients to face-to-face appointments at PHC centres or specialist facilities. Funding for the helpline came from the governments of Denmark and Canada.
Educating patients about COVID-19 and the continuation of NCD care was primarily achieved through television and social media. Meanwhile, 71, 000 patients who were subscribed to an SMS service as part of the “end diabetes” project, were sent information on COVID-19 from WHO.
Other actions included:
Many of these successful policies – such as those on digital health and telemedicine – will be continued after the pandemic and have helped to build infrastructure and partnerships for the future.
The National Mental Health Programme led the development and implementation of a multisectoral plan to make mental health teams part of the COVID-19 emergency response.
The programme was able to:
The continued provision of mental health and psychosocial support services gave Sudan the opportunity to incorporate them into humanitarian response efforts, as tens of thousands of additional refugees entered Sudan from Ethiopia during the pandemic. Although one in five refugees is likely to have a mental health disorder, these are often overlooked by humanitarian assistance programmes.
Sudan worked with WHO and UNHCR to create an approach to refugee mental health and psychosocial support services with 3 core elements:
This approach, with mental health and psychosocial support built into the response, gave vulnerable people the essential treatments they needed, but also helped to strengthen Sudan’s national mental health system.
This country story is part of a series on sharing successful strategies from the Eastern Mediterranean Region mitigating noncommunicable diseases and mental health disorders during the COVID-19 pandemic and beyond. Discover additional stories and insights in the full report published by the World Health Organization Regional Office for the Eastern Mediterranean.