World Health Organization
Multistakeholder action to improve health and wellbeing by reducing health inequity through the first Healthy Island initiative in the Eastern Mediterranean Region
23 Oct 2023
World Health Organization. Regional Office for the Eastern Mediterranean | 08 Sep 2023
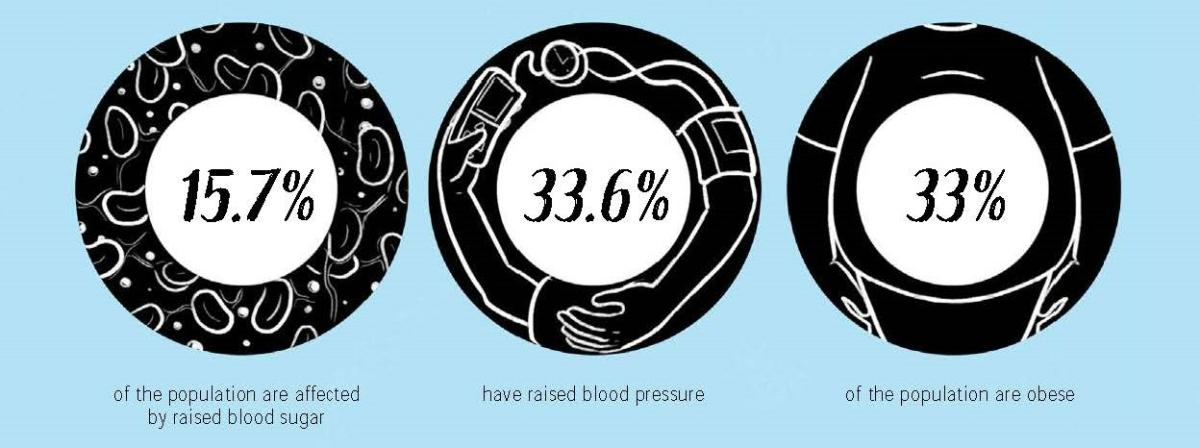
Noncommunicable diseases (NCDs) account for 72% of deaths in Oman, with almost one third of the population suffering from high blood pressure. Most people living with NCDs receive health services through primary health care centres. Oman worked quickly and effectively to adapt primary health care services to meet the sudden pressure of COVID-19 and to continue providing NCD services while integrating remote technologies. These technologies can continue to be used after the pandemic.
Oman banned the public use of waterpipes in March 2020. This was reinforced with an extensive awareness-raising campaign, mainly via Facebook and Twitter.
World No Tobacco Day 2020 – The Ministry of Health released video clips at peak TV viewing times linking tobacco use to the transmission of COVID-19.
In 1996, the Ministry of Commerce, at the request of the Ministry of Health, mandated the fortification of wheat flour with iron and folic acid. This strategy continues to reduce the occurrence of spina bifida.
The Ministry of Health is working with other ministries and partners to promote sustainable food systems. Strategies include increasing local production and consumption of fruits, vegetables and fish.
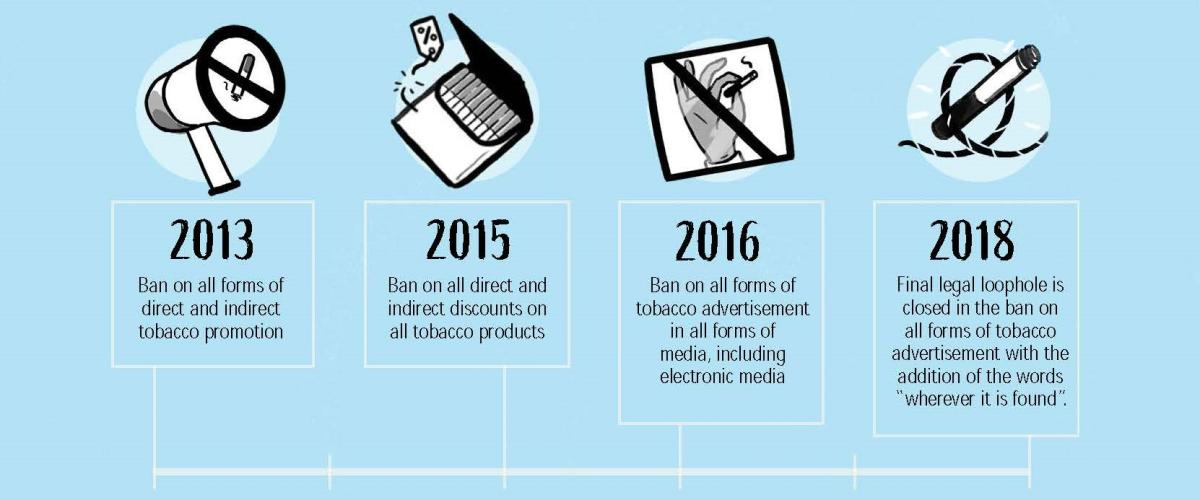
Between 2013 and 2018, Oman adopted a comprehensive ban on tobacco advertising and promotion. The National Committee for Tobacco Control, including the Ministry of Information, the Ministry of Commerce, Industry and Investment Promotion, the National Coordinating Mechanism and local municipalities worked closely together over five years to enact the ban.
They worked step by step to close off all legal loopholes that could be exploited by tobacco companies.
This success was only made possible through concerted multisectoral collaboration. Oman has shown that by taking carefully thought-out steps, every country can make significant progress on their journey to 2030.
When the COVID-19 pandemic hit, the Ministry of Health reassigned many primary health care (PHC) centres to the management and treatment of COVID-19 patients. As a result, authorities rearranged health services for people living with NCDs, most of whom were being treated at PHC centres.
These primary health care centres triaged patients with NCDs according to how well controlled their conditions were in order to identify the best way to treat their needs. Centres then offered remote health services to those living with controlled NCDs through telemedicine and mHealth, primarily by way of phone consultations, and collaborated with volunteers to deliver medicines to patients’ homes.
Other remote services included:
The Ministry of Health undertook two rapid assessments of the new remote services, to see whether they were meeting patients’ needs. The findings of these assessments helped the Ministry of Health to adapt the services to improve access. Further changes included:
The 2017 STEPS survey in Oman revealed that:
As primary health care is the first point of entry to health services for most patients in Oman, the Ministry of Health acted to strengthen and equip PHC facilities to prevent, screen and manage NCDs. The National Non-Communicable Diseases Screening Programme was integrated into PHC centres which were given standardized disease registers for diabetes, hypertension and asthma, so that chronic disease clinics could be monitored. Patients are now registered in these clinics when they are diagnosed and given booklets to record follow-ups and medication.
The disease registers collect a range of information about the patients and help the Ministry of Health to:
As well as the benefit of high-quality data driving better decision-making, the primary care surveillance system has also led to improvements such as new medicines being provided at PHC level and the introduction of well-being and obesity clinics.
Work is underway to convert the system to an electronic register, while future developments could include adding data from the private health sector to give an even clearer picture of the total burden of NCDs in the country.
Oman made mental health a central pillar of its COVID-19 response and worked to mitigate the psychological consequences of the pandemic, such as isolation, fear and stigmatization.
The Ministry of Health developed guidelines on managing mental health, while the public and private sectors used virtual technology and social networks to promote good mental health and ensure continuity of care during the pandemic.
Smartphone apps aimed at reducing stress, such as Nafas, offer guided meditations in Arabic, while helplines such as “Not Alone” provide support to anyone experiencing mental health issues including depression, anxiety and suicidal thoughts. During the pandemic, the Ministry of Health and the Ministry of Information collaborated to broadcast advice on mental health issues from experts via radio and television.
Outpatient services were adapted to prioritize emergency cases and those needing close follow-up to stabilize their conditions, while stable patients were given two to three months of medication.
Psychiatric clinics also liaised with PHC facilities to provide psychosocial support services.
This country story is part of a series on sharing successful strategies from the Eastern Mediterranean Region mitigating noncommunicable diseases and mental health disorders during the COVID-19 pandemic and beyond. Discover additional stories and insights in the full report published by the World Health Organization Regional Office for the Eastern Mediterranean.